This course is part of the RCOG Core Knowledge series.
Sexual assault is common with 1 in 4 women having been raped or sexually assaulted as an adult. Disclosure of sexual assault however continues to be low. The Crime Survey in England and Wales (2018) revealed that only 17% of people who had experienced a sexual assault had reported it to the police. Embarrassment and the fear of further humiliation were listed as barriers for disclosure.
Sexual assault can have various presentations to healthcare professionals. Patients often present with acute injuries, but do not immediately disclose the causative sexual assault. Some patient will never disclose a sexual assault unless directly asked, and so for the medical professional that sees them, knowing when to appropriately include it in a list of differentials can be key.
There are many barriers for disclosure and reporting. It is therefore important that on disclosure of sexual assault being met with a supportive and non-judgemental approach and being believed is crucial to that individual's journey.
Most units will have a protocol for sexual assault and rape, but it is often not read or highlighted to new staff. Increasingly, many areas have Sexual Assault Referral Centres (SARCs). However, access to these services and the availability for long-term follow-up is variable between regions. It is, therefore, important to familiarise yourself with local policies and their services.
There is often a hesitance among healthcare professionals to address and medically manage sexual assault. This comes from a lack of training and a fear of contamination of forensic evidence and causing harm to any future legal case that may arise. It is vital to remember that the primary concern should always be the immediate treatment of injuries and offering appropriate and timely medical care.
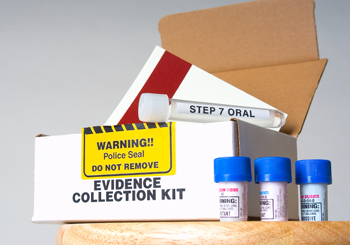
This course will provide some knowledge and information on how to best preserve forensic evidence while providing timely medical care for sexual assault victims.
Where there is an absence of injuries and medical aftercare has been addressed, it is appropriate to seek advice from a local sexual assault referral centre as the forensic medical examination is best carried out by a trained forensic practitioner.
When you have completed this course you will be able to:
- demonstrate an understanding of the law relating to sexual offences and the current issues affecting disclosure and reporting of sexual assault
- provide appropriate management when someone reports that they have experienced a sexual assault
- describe the basic principles of a forensic medical examination
- to be able to document findings and take early evidence where necessary
- describe injury types using appropriate forensic terminology
- demonstrate knowledge of the long-term consequences arising from sexual assault
Dr Nisha Krishnan MRCOG (2013, 2017, 2019, 2023)
Dr Krishnan is a consultant obstetrician with a special interest in high risk obstetrics, perinatal mental health and trauma informed care. She has a special interest in Forensic Gynaecology after she took 1 year out of programme for a clinical fellow post at The Havens (London-based sexual assault referral centre) and continued to do out of hours work alongside her training. Having worked as a consultant obstetrician for the last 5 years, has resumed her work in forensic gynaecology in Scotland. She currently works as a sexual offences examiner at the West of Scotland Sexual assault referral centre (Archway). In the past, she has also volunteered at Freedom From Torture, an organisation for the survivors of torture, where she worked as a team assessment doctor, as well as produced medico-legal reports for survivors of torture. This gave her the experience of working in a multidisciplinary team dealing with both the physical and psychological sequelae following sexual assault and trauma.
The content of this course relates to the following Capabilities in Practice (CiPs) and key skills:
CiP 1: Clinical skills and patient care
Relevant to all key skills
CiP 2: Working in health organisations
Relevant to all key skills
CiP 3: Leadership
Influences and negotiates
Leadership skills
Demonstrates insight
Effective use of resources
CiP 5: Human factors
Relevant to all key skills
CiP 6: Developing self & others
Relevant to all key skills
CiP 8: Educator
Effective teaching
Interprofessional learning
Supervises and appraises
CiP 9: Emergency gynaecology and early pregnancy
Manages non-pregnancy pelvic pain
Manages non-pregnancy vaginal bleeding
Manages acute infections
Manages complications of treatment
CiP 11: Non-emergency gynaecology and early pregnancy
Manages sexual wellbeing
CiP 13: Non-discrimination and inclusion
Relevant to all key skills
CiP 14: Health promotion
Relevant to all key skills
Further details about each CiP can be found within the O&G Core Curriculum 2024 Definitive Document, available here.
Product Details:
Product Name
Price
Rape and forensic gynaecology - 12 Month Access
£64.80
Login to purchase
| Product Name | Price | |
| Rape and forensic gynaecology - 12 Month Access | £64.80 | Login to purchase |