This course is part of the RCOG Core Knowledge series.
The RCOG recommends that hospitals provide a dedicated one-stop menstrual disorder clinic. Similarly, the UK Department of Health recommends hospitals provide a rapid access clinic to enable specialist review of suspected gynaecological cancer pathology within 2 weeks of general practitioner (GP) referral.
Ideally, both clinics should have facilities for outpatient diagnostic gynaecology, including hysteroscopy, colposcopy and pelvic ultrasound. Given the overlapping skill sets, it seems likely that in the future such clinic services could be offered in a combined one-stop menstrual disorder clinic, with some services led by specialist nurses. Such an approach would help to achieve NHS operational ‘referral to treatment’ standards (62 days for urgent GP referrals and 126 days for non-urgent GP referrals) and has potential to achieve NHS cost savings.
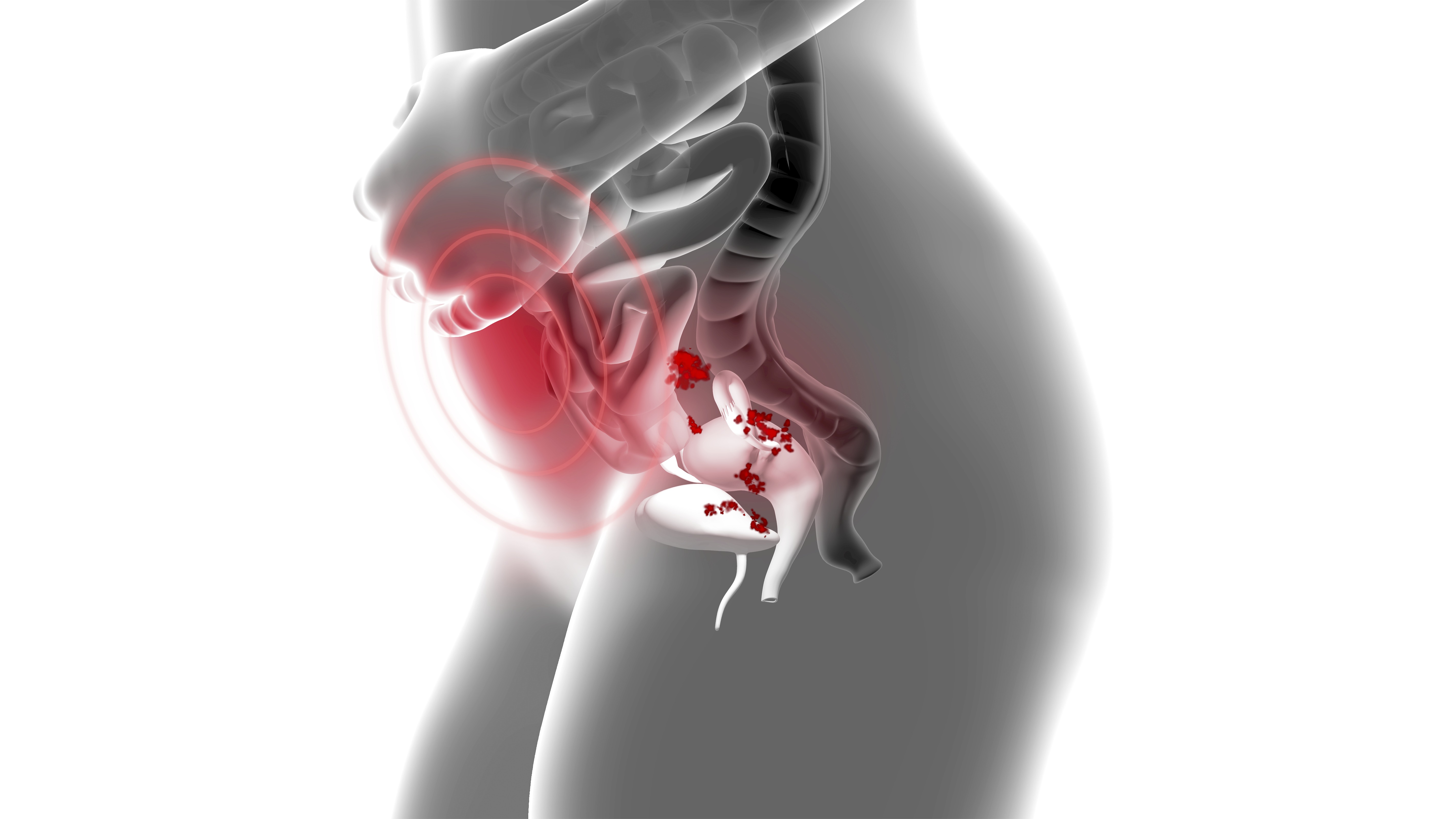
This course provides you with comprehensive, up-to-date and evidence-based information on how to manage women with abnormal uterine bleeding (AUB) and how to deliver an effective one-stop menstrual disorder clinical service.
When you have completed this course, you will be able to:
- demonstrate knowledge of AUB terminology and the FIGO classification system (PALM-COEIN) for causes of AUB and understand the risks and benefits of treatment options
- identify ‘red flag’ features requiring secondary care referral
- describe the principles of uterine and endometrial assessment using pelvic ultrasound, endometrial biopsy and hysteroscopy and identify the indications for using other imaging modalities in selected groups
- interpret the hierarchical three-step treatment approach for HMB
- recognise the risks and benefits of: operative hysteroscopic procedures, endometrial ablation, uterine artery embolisation and MRI-guided focused ultrasound ablation
- counsel women on treatment options explaining the nature, risks and benefits of medical and surgical treatments
- recognise the need for appropriate referral for more complex cases for detailed evaluation
- use appropriate referral pathways and local protocols if AUB or abnormal findings are identified.
Dr Rohan Chodankar (2014, 2016, 2019, 2024)
Dr Rohan Chodankar is Single Best Answer Lead, Gynaecology, on the eLearning Core Knowledge Editorial Board.
Dr Anna King (2024)
Dr Anna King MRCOG is a current Senior Specialty Trainee in Obstetrics and Gynaecology in South East Scotland.
The content of this course relates to the following Capabilities in Practice (CiPs) and key skills:
CiP 1: Clinical skills and patient care
All key skills covered
CiP 3: Leadership
Effective use of resources
CiP 6: Developing self & others
Commits to continued learning
CiP 11: Non-emergency gynaecology and early pregnancy
Manages abnormal vaginal bleeding
Further details about each CiP can be found within the O&G Core Curriculum 2024 Definitive Document, available here.
Product Details:
Product Name
Price
Abnormal uterine bleeding - 12 Month Access
£64.80
Login to purchase
| Product Name | Price | |
| Abnormal uterine bleeding - 12 Month Access | £64.80 | Login to purchase |